Blood Pathogen Panel (BPP)
Introduction
The Blood Culture ID (BCID) Multiplex PCR testing went live on June 23, 2021.
- This test is ordered by the laboratory staff when a blood culture is positive from our instrument.
- The result for each organisms appears as: “Detected” or “Not Detected.”
- The FilmArray BCID Panel is a multiplexed nucleic acid test intended for use with the FilmArray Instrument for the simultaneous qualitative detection and identification of multiple bacterial and fungal nucleic acids in positive blood culture samples. The following gram-positive bacteria, gram-negative bacteria, and yeast are identified using the FilmArray BCID Panel:
- Gram-Positive Bacteria
- Enterococcus
- Listeria monocytogenes
- Staphylococcus
- Staphylococcus aureus
- Streptococcus
- Streptococcus agalactiae
- Streptococcus pneumonia
- Streptococcus pyogenes
- Gram-Negative Bacteria
- Acinetobacter baumannii
- Enterobacteriaceae
- Enterobacter cloacae complex
- Escherichia coli
- Klebsiella oxytoca
- Klebsiella pneumonia
- Serratia marcescens
- Proteus
- Haemophilus influenzae
- Neisseria meningitidis (encapsulated)
- Pseudomonas aeruginosa
- Yeast
- Candida albicans
- Candida glabrata
- Candida krusei
- Candida parapsilosis
- Candida tropicalis
- Gram-Positive Bacteria
- The FilmArray BCID Panel also contains assays for the detection of genetic determinants of resistance to methicillin (mecA), vancomycin (vanA and vanB), and carbapenems (blaKPC) to aid in the identification of potentially antimicrobial resistant organisms in positive blood culture samples.
- Antimicrobial resistance genes
- mecA – methicillin resistance
- vanA/B – vancomycin resistance
- KPC – carbapenem resistance
- Antimicrobial resistance genes
- Limitations of the test:
- The FilmArray BCID Panel may not distinguish mixed cultures when two or more species of the same genus or organism group are present in a specimen (e.g., S. aureus and S. epidermidis).
- This test is a qualitative test and does not provide a quantitative value for the organism(s) in the sample.
- The FilmArray BCID Panel does not contain assays for obligate anaerobic organisms that might be recovered in blood culture.
- Results from this test must be correlated with the clinical history, epidemiological data, and other data available to the clinician evaluating the patient.
- The FilmArray BCID Panel does not detect all species in the Enterobacteriaceae family. Morganella spp., Providencia spp., Rahnella spp., and Yersinia spp. will not be detected.
- Based on sequence analysis, the FilmArray BCID Panel may not detect S. pneumoniae serotypes 11A and 19, or may detect these serotypes with reduced sensitivity compared to other serotypes.
- The FilmArray BCID Panel will not detect encapsulated Neisseria meningitidis containing the variant ctrA gene sequences.
- The FilmArray BCID Panel does not detect all species of Enterococcus, Proteus, Staphylococcus or Streptococcus.
- We have provided a YKHC BCID Badge Buddy for providers. Please use these to help you interpret the BCID results.
YKHC Rapid Blood Pathogen Identification Panel Guideline
(last updated 6/2021)
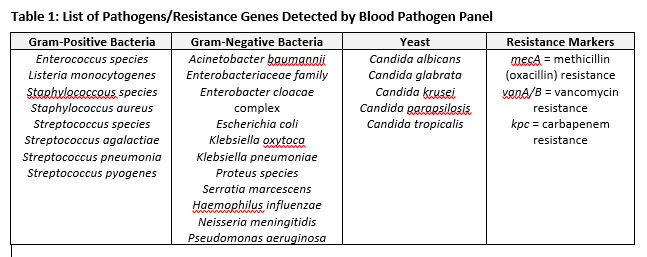
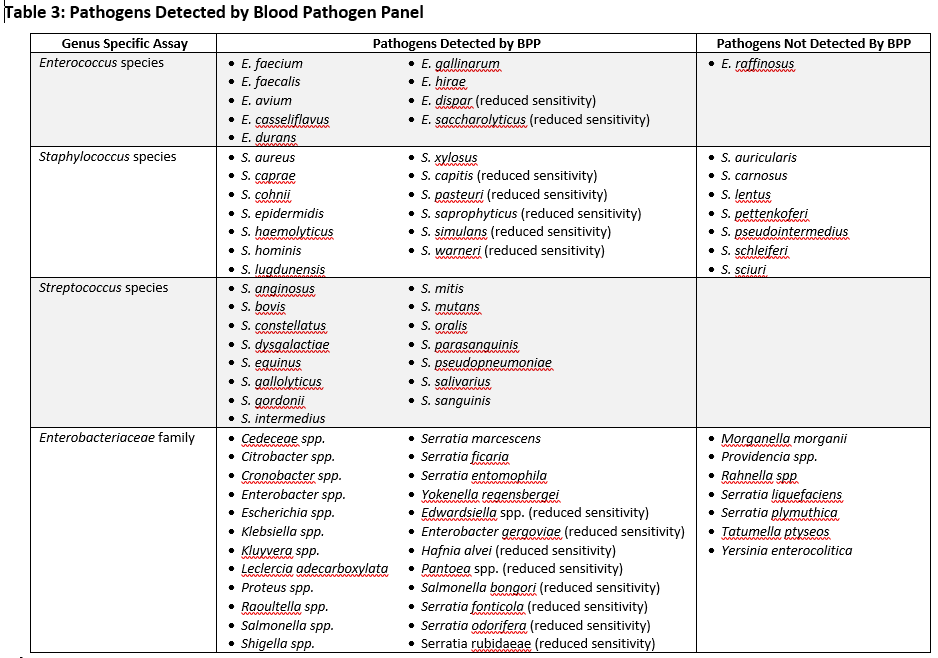
YKHC utilizes an FDA approved test called the Blood Pathogen Panel (BPP) performed on the BioFire BCID instrument. The test uses polymerase chain reaction (PCR) to amplify DNA targets from 3 groups of pathogens (gram positive bacteria, gram negative bacteria and yeast). It is performed directly following a positive blood culture and allows rapid identification of 21 different pathogens (Table 1). It also detects genes responsible for vancomycin-resistant Enterococci, methicillin-resistant Staphylococci and one of the genes responsible for carbapenem-resistant Enterobacteriaceae. In addition to detecting multiple species-specific assays, the panel also contains 4 genus specific assays (Enterococcus, Staphylococcus, Streptococcus and Enterobacteriaceae) that allows detection of pathogens for which there are no specific targets. A comprehensive list of all pathogens detected by BCID can be found in Table 3.
Immediately following a positive blood culture, the YKHC microbiology lab performs the BPP. The results from the panel (pathogen identification) are typically available within 2 hours. It is important to note, that this test is NOT a standalone test. Blood samples with bacterial growth are still cultured and proper MIC testing is performed. The rapid reporting of pathogen identification allows for early escalation or de-escalation of antimicrobials to the most appropriate therapy while waiting for susceptibilities. A list of recommended antimicrobial treatment choices are outlined in Table 2.
The YKHC Antimicrobial Stewardship Program (ASP) developed these recommendations in collaboration with ANMC Infectious Diseases based upon the institutional antibiogram and national guidelines issued by the Infectious Diseases Society of America (IDSA). Relevant local susceptibility data is provided for gram-negative pathogens if activity for the antimicrobial is available. When both blood culture gram-stain and BPP results are available, current antimicrobial therapy should be evaluated in light of the clinical picture and adjusted to the most appropriate regimen. Additionally, when full susceptibility results become available therapy should again be evaluated and adjusted to the most appropriate narrow spectrum agent. It is important to note that certain infections are often polymicrobial in nature. In most cases, isolation of a single pathogen from the BPP should warrant narrowing of antimicrobial therapy, but should never result in over-narrowing. An example would be in complicated intra-abdominal infections where anaerobes are frequently present and therapy against these pathogens should generally be included until definitive cultures of the site of infection are available. Providers must use clinical judgment on a case-by-case basis.
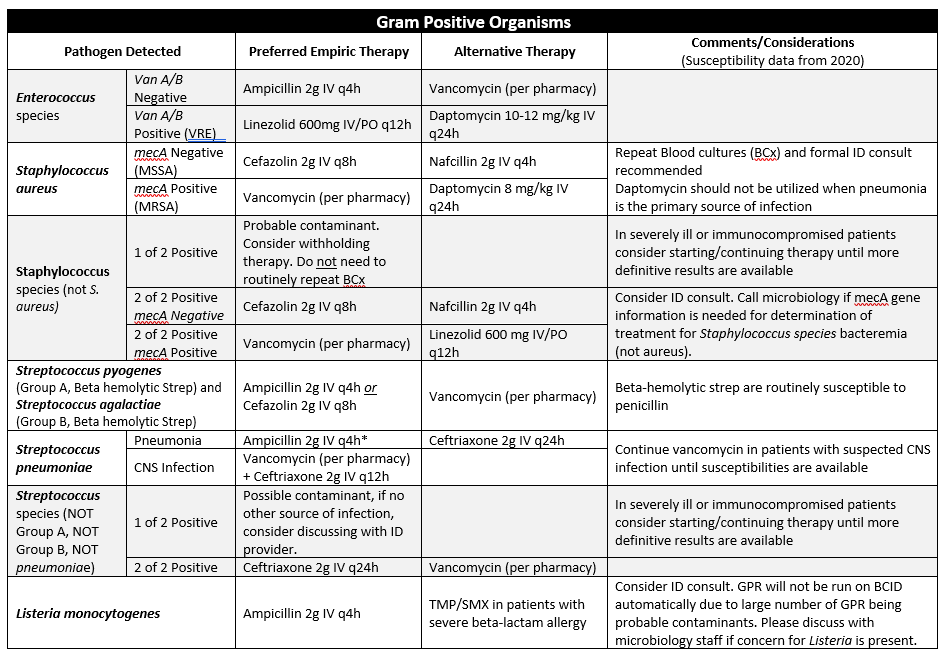
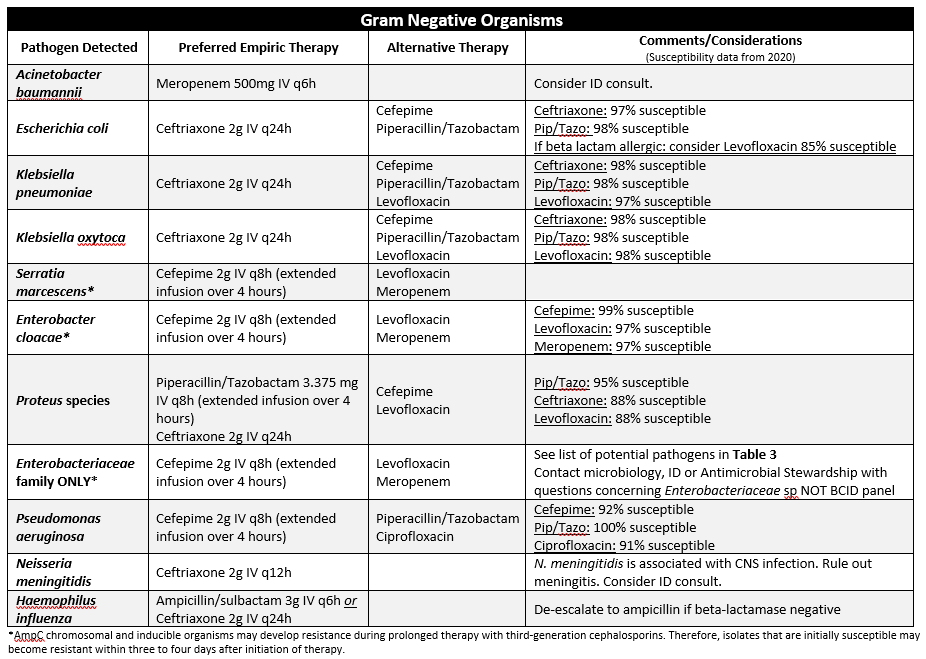
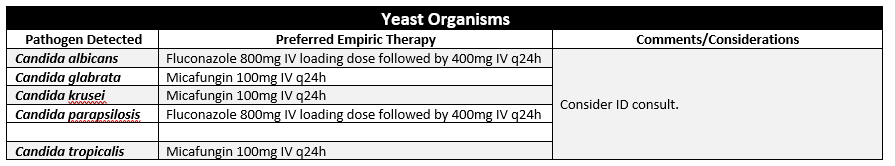
Table 2: Blood Pathogen Panel Results and Recommended Empiric Therapy
The table below contains interpretations of BPP data and recommended empiric antibiotic therapy for treating blood stream infections (BSIs) at YKHC. When the clinical picture and judgement dictates, patients who respond to narrow spectrum therapy do not always need to be escalated, even if this guideline recommends a broader spectrum agent. Similarly, patients who continue to deteriorate or are not clinically responding despite appropriate empirical antimicrobial therapy may require broader coverage. Allergies, organ dysfunction and history of multi-drug resistant organisms (MDROs) should always be considered prior to selecting empiric antimicrobial therapy. Data on susceptibility for the various gram-negative pathogens is derived from the 2020 institutional antibiogram.
References
- Schooneveld T, Bergman S, Fey P, et al. Recommendations Regarding Use of Rapid Blood Pathogen Identification Panel Data. Nebraska Medicine. 2017
- Banerjee R, Teng CB, Cunningham SA, et al. Randomized Trial of Rapid Multiplex Polymerase Chain Reaction-Based Blood Culture Identification and Susceptibility Testing. CID 2015;61(7):1071-80. Doi: 10.1093/cid/civ447
- Bookstaver PB, Nimmich EB, Smith III TJ, et al. Cumulative Effect of an Antimicrobial Stewardship and Rapid Diagnostic Testing Bundle on Early Streamlining of Antimicrobial Therapy in Gram-Negative Bloodstream Infections. AAC 2017;61(9):e00189-17