Category:SRC Clinic Provider Orientation
Overview
YKHC now operates five Community Health Centers based in Aniak, Emmonak, St. Mary’s, Hooper Bay and Toksook Bay. Each Subregional clinic is a hub for its surrounding villages for economics and transportation services. Subregional clinics (SRCs) located in strategic areas of the Yukon-Kuskokwim Delta serve as referral centers for villages with the greatest need for services and access to higher levels of care. Sites were chosen based on careful analysis of village-based service data, strategic location, and ability to support the clinics.The goals of these clinics are to promote health, prevent disease, and bring higher quality health care, primary and social services closer to needy families and their home environment.
SRCs are designed to provide basic, essential health care as well as behavioral health services, which include mental health and substance prevention services. Each SRC is staffed to provide primary care, chronic care follow-up, emergency stabilization and transport, routine lab and x-ray procedures, limited specialty care, basic dental services, substance abuse counseling and support, and mental health services. Additional services to the region include EPSDT physicals, Head Start and kindergarten physicals, sports physicals, physicals for active duty army National Guard personnel as well as drug testing for employment personnel.
Staffing
Routine services are provided during scheduled clinic hours. After hours, community health aides provide education and treatment and a midlevel provider is available for emergency care, which falls outside the scope of practice for CHA/Ps. The following staff are recruited and trained to be on site at each SRC, Nurse Practitioner/Physician Assistants, community health aides, nursing assistants, dentist, DHAT, dentist assistant, lab technician, radiology technician, community health representative, behavioral health clinician, wellness counselor, manager and ancillary staff to support day-to-day operations. Itinerant staff also provide services on a rotating basis depending on the needs of the community to include but not limited to physical therapy TDY mid-level practitioners, orthopedics, mammography, optometrists, physicians, audiologist, and child psychiatrist.
Training for Local Hire
With the drive within the corporation to develop culturally relevant programs for primary care and foster Native self Determination in the control and management of health delivery, training programs have been established to train local people to staff the SRCs. Laboratory technicians are locally hired employees who work on a training program though the University of Alaska to prepare them for phlebotomist up to a Medical laboratory Technician with minimal travel outside their village. There is a similar model for Certified Coders. They are hired locally and are provided with some off-site didactic training and then use modules from the Internet to prepare them for the State Certified Coding Exam. This has been supplemented with the Community Health Center Coding Training provided by the National Association of Community Health Centers. Other training programs taking into account cultural aspects are the radiology technician, dental assistant and dental hygienist. These employees are also hired locally and trained to follow established guidelines and protocols.
Health Aide Responsibilities
Community Health aides function as primary acute care providers but are expanding services to provide increasing levels of health promotion and disease prevention. Training on EPSDT physicals for age 0–20 has been completed. The Operations Manager provides immediate supervision of employees who work in the clinic and coordinate services between providers. The intention is to provide enough flexibility in management, staffing and day-to-day operations to permit dynamic changes and expansion in services to meet the needs of each SRC community.
Specialty Visits
Along with regular on-site clinics other specialty clinics that are provided at SRC include regular optometry visit for contact and glasses fittings and quarterly physical therapist visits. Portable mammogram clinics are scheduled at each Subregional Clinic. So are Diabetic clinics for “one stop care” for diabetics in the region. Other specialty clinics include audiology and colonoscopy.
Links
Map of Subregional Clinic service areas in the YK Delta
Subregional Clinic Guide
Clinic Description
We have five subregional clinics (SRCs): Aniak, Emmonak, Hooper Bay, St. Mary’s, and Toksook Bay. See Map. Each clinic has enhanced resources and capabilities compared to regular village clinics. Each clinic has radiological imaging, lab facilities and limited ER/Urgent Care equipment.
In terms of staffing, the goal is to have two midlevel providers plus behavioral and dental health aides to provide care to patients in the SRC village as well as those villages in close proximity. At times the SRC may be the staging area for emergent transports that are not able to make it to Bethel, en route to Anchorage. Midlevel providers care for patients during regular clinic hours as well as provide nighttime and weekend call for emergencies.
Midlevel providers function like specialists in the region. They are called upon to provide care involving many different disciplines such as orthopedics, women’s health, acute pediatric issues, and trauma resuscitation. We have medical specialists such as cardiology, neurology, internal medicine, etc. in Anchorage, which can be contacted for consults. Pediatric, Emergency and Family medicine providers are available in Bethel for consults. Please don’t hesitate to call for any acute issues in which you need assistance.
Remember there are YKHC Clinical Guidelines for reference on many clinical situations. They lay out specific medical plans based on our population's challenging illnesses and our specific antibiotic resistance patterns.
Remember that health aides in villages may have already prescreened 50 percent of the patients we see and only the sicker ones have been sent on to the SRC. Therefore at times you need to be more aggressive with our sick patients.
Job Description/Duties
ON CALL
You will be seeing patients during the day, but on call on nights and weekends for emergencies. Our health aides will be on first call but will call you if they need additional help or approval of their plan. You may not have to come in but you need to be available to talk to them. Some SRCs have working cell phones to make this easier. Some villages (Aniak at this point) have a working ambulance that will bring patients directly to the clinic for you to see.
If you are the only provider at a SRC you will be on call Monday, Thursday with the weekends off except for dire emergencies.
It is important for the Health Aides to take first call and to fully assess the patient, then give you a call unless there is a dire emergency. That is their duty. Please encourage the health aides to do the initial assessments. When there is a seriously ill patient all health aides and staff may be called in to assist with that patient.
Required and Recommended Meetings
Note: Meetings can be arranged via teleconferencing from the SRCs
General Clinic Information For SRC Reference
Preparing For and Navigating Daily Clinics
Clinic Appointments/Encounters
SRC Specific Information
Admissions/ER Management/Need To Transfer
If you are seeing a patient you feel needs to be admitted to Bethel or is too sick for SRC management, the patient will need to be Medevaced from the SRC to either Bethel or Anchorage for a higher of level of care.
- Contact either Inpatient Provider Yukon /Kusko or ED Physician, depending on case and decide on the medevac plan.
- Determine where the patient needs to be transferred- Bethel or Anchorage.
- Determine who will activate LifeMed .
- Obtain Medevac Packet which contains consent forms which need to be completed
- Complete your RAVEN documentation
Some things to keep in mind:
Escorts can fly with the patient if there is room, but YKHC will not pay for them to fly home, so their travel home will be out of their own pocket.
Any time you initiate a Medevac know that you will be talking to several different people and making several different calls.
If they are flying directly to Anchorage from a SRC, the SRC provider will be the one calling for a direct accepting physician in the receiving hospital. You will call either the ER of Providence or Alaska Regional if it is a non-beneficiary patient or at ANMC the ortho or surgery or internal medicine physician. Explain the case to them and why you're medevacing the patient. Once they accept, you place their name and the place of transfer on the PTO Patient order form. You need to notify the YKHC ER just so they know that a medevac is coming from Anchorage to your village, but you can do all the communication, etc. yourself.
If flying to Bethel, usually the accepting physician is the Ward doctor, or the ER doctor will fill out the PTO and be the accepting.
If the patient is going to Anchorage you will then get two more calls. One is from the house supervisor at the accepting hospital, usually a nurse who wants to verify the patients name and diagnosis.
You will also receive a call from the LifeMed medical control, which is based in Anchorage to ask about the patient's condition, etc. before the paramedics who pick up the patient take over control.
Bethel has an OR that can be used for emergencies, but no ICU and no general surgeon or neurosurgeon. Bethel has a CT scan but no MRI. Depending on which village you are in, you may be able to call for an ANMC medevac, if immediate surgery or a vent is needed, but talk to the Bethel doc to help you make that call.
The types of admissions for YKHC hospital are mainly large abscesses and/or cellulitis that have failed outpatient treatment, large lower extremity cellulitis/abscesses that have not yet had outpatient treatment, pneumonia, bronchiolitis, suicidal ideation, COPD exacerbation, fever in a neonate and labor.
If you have a child that is not a Chronic Peds Patient (which you can tell by looking at the banner on the first page of the patient’s health summary) he or she can be admitted to the Family Medicine Ward doctor. If it is a complicated child and/or it is a Chronic Peds Patient, the child should be discussed and possibly admitted to the Pediatrician on Call. Page On Call Peds using the pager sytem on Raven. The pediatricians always help with the treatment and plan of care for the Chronic Peds Patients.
Medevacs SRC Paperwork and Process
At times you will have a patient arrive who is too sick to stay at the SRC. You will need to care for the patient and initiate a medevac. Evaluate the patient, have the health aide start your treatment plan—i.e. start an IV and bolus fluids, and call the ER to consult and initiate the medevac. Once the ER agrees, you can call the Anchorage dispatch center, 800-478-5433 and they will call the Bethel crew to get ready and come, or the ER can do that for you. If there are weather delays, the dispatch center will let you know. You will have to handle the patient until the Medevac comes, which is a plane with two paramedics and much equipment.
There is a consent form, and a Patient Transfer Order Form you will need to fill out. I really recommend that you use your PCC, but then document all vitals, your secondary exam on extra pages and the flow sheet. If you are able to write a transfer summary, that is helpful, but not essential. All meds need to be documented. Before the patient is handed off to the Medevac crew you need to do a second exam and document how the patient is doing. You also need to document the time that the medevac is initiated and that the physician was consulted with, what time the team arrived and what time they left.
At times the patient is so severely ill or damaged that you know that they will need to go directly to Anchorage if possible. If you are in St. Mary’s, Aniak, or Emmonak, that may be possible. If the patient is going to need surgery, i.e. a gunshot wound, or is already intubated it may make more sense for them to go straight to ANMC. Discuss it with the Bethel ER and they or you can contact ANMC directly, talk to the surgeon or internal medicine MD and get it initiated. If that happens, the nurse supervisor from ANMC should call you within 10-30 minutes to say they have sent the medevac. If that doesn’t happen, call ANMC back to make sure it is on its way.
Sometimes the patient has been stabilized and time is of the essence and the medevac team may ask you to do a runway transfer, bringing the patient to the runway for quicker turnaround time. If this is the case, get a copy of all paperwork to give the team and get them to the runway.
Example of Good Medevac Documentation
Births
All pregnant women are supposed to leave the village one month prior to their due date, this date is called their Be in Bethel date. Occasionally this doesn’t happen. If it doesn’t, you may be called upon to deliver a baby in an emergency.
- Call the Ward Doctor on Call for consultation.
- Turn on the infant warmer located in Trauma Bay
- Call for additional help, probably at least one of the health aides there has delivered a baby.
- Turn on Oxygen and Suction,
- Prepare Vitamin K and Hepatitis B for the baby.
- Document a note for the Mother as well as infant in RAVEN once they have been registered in the system.
- Take a deep breath> You can do it!!
- Contact Pediatrics on Call for any pediatric questions.
Once the baby delivers it will need a 1 minute and a 5 minute Apgar score. Wipe off the baby for a few seconds and then get rid of the wet blanket and put a fresh preferably warm one on the baby. If the baby is doing OK, mom’s chest is an ideal place for the baby to be.
Once things settle down, give the baby a Vitamin K shot. Mom and baby will probably be traveling by commercial or medevac plane to Bethel, as both need to be observed—baby for 48 hours.
Death in Village
People do die in the village. When this occurs they will need a provider to pronounce them dead and document it and call the State Troopers/VPSO and the Medical Examiner and North Wing Provider on call, so they can start the paperwork process and death certificate.
If this was an expected death, an Expected Home Death form can be filled out ahead of time and faxed to the State Troopers and the Medical Examiner, making it very simple on the day of the actual death.
If this was not done, you will need to have more details for the officers and ME. Go to the scene of the demised patient, call him using his/her name, examine her eyes, feel for breath, and listen for breath sounds and heartbeat for approximately 30 seconds. If nothing, he is officially pronounced dead at that time.
Document this visit with the history of the patient and the above exam. Notify
- The State Troopers, 543-2294 in Bethel
- Medical Examiner, 1-888- 332-3273.
- North Wing Doc 907-543-6300.
- Life Alaska 1-888-543-3287 – Get a case reference # and write it on your documentation
Example of a Good Free Text Death Note
I was called by the nurse to examine the patient to pronounce death. The patient was found to be apneic and pulseless with no cardiac activity at 1910 after being weaned off of dobutamine for end-stage cardiomyopathy. He had been comfortable since that occurred with a PCA pump. I examined him 1927 and found that he was pulseless apneic and had no cardiac activity. Pronounced dead with the time of death at 1910. Cause of death cardiomyopathy.
There are numerous family members present and they were informed. They were appreciative of the opportunity to have him back here in Bethel surrounded by friends and family.
Contacted State Troopers and notified them.
Contacted the Medical Examiner and notified them.
Contacted the North Wing on Call in Bethel to get HIS working on the death certificate.
Contacted Life Alaska – pt not a candidate for organ donation – Case # 00000.
Pediatrics
We have a pediatrician on call every day for the inpatient PEDs patients. The on-call PEDs takes consults. You will see many children with respiratory illnesses. Children 90 days and under, who have a fever of 100.4 or higher, or with any source of infection such as otitis media or pneumonia will need to be seen by the ER for a septic work up. On some occasions, during Radio Medical Traffic (RMT), for a child under the age of three months and if the Health Aide suspects an OM, do not treat with antibiotics. Have the infant sent to Bethel emergency room for evaluation. We do not give antibiotics to children under 90 days without having them evaluated in Bethel.
There is quite a bit of respiratory illnesses in the Delta region with bronchiolitis and pneumonia. Kids with wheezing and rhinorrhea that have a reassuring respiratory exam that is most likely bronchiolitis, can be given saline/albuterol nebs in the village and followed closely. We do not routinely give steroids for bronchiolitis. If you are giving nebs more than Q 4 hours in the village, the child must come in for evaluation.
See our Pediatric Guidelines. In particular be sure to look at all the respiratory, OM, UTI and Seizure Guidelines.
Remember the first line antibiotics for OM is amoxicillin; watchful waiting is an opyion for most kids and use drops whenever possible if there are only draining ears.
Kids with culture proven UTI, need treatment for their UTI once the culture results are back. If the patient is stable, they will not get ABX until the cx results are back. See the new pediatric UTI guideline. Remember that dysuria without urgency and increased frequency, in the 2-7 year old patients, is most often due to vulvovaginitis and can be treated with sitz baths, A&D ointment and improved hygiene.
Chronic Pediatric Patients
We have a pediatrician on call every day for the inpatient peds patients and for consults. A Chronic Pediatric Patient is a complicated kid, who may be a preemie, or twin, or have a chronic serious illness that is being managed by a pediatrician. If you see a Chronic Pediatric Patient in the SRC, you must consult the Peds on call for a treatment plan before the child leaves the building. You can tell a patient is a chronic peds patient by looking at their problem list under the registries and seeing Chronic Peds. You can also tell by looking at their sticker and seeing if they have a pediatrician listed for their pod. If it is an animal, bird, or fish pod name they are not chronic peds.
You can contact them by calling the operator, 0, and asking them to page them.
You will see many children with respiratory illness. Children 90 days and under who have a fever 100.4 or higher, or any source of infection, such as otitis media or pneumonia, need to be seen by the ER for a septic work up. On Radio Medical Traffic, if the Health Aides suspects an OM in a child under 90 days, do not treat with antibiotics Have the infant sent to Bethel emergency room for evaluation. We do not give antibiotics to children under 90 days without having them evaluated in Bethel.
Kids with a Cath proven UTI need treatment for their UTI and then look at the Peds UTI guidelines to see what the next steps are.
Lab
Labs in Bethel include cultures, comprehensive chemistries, CBC, etc. Viral loads and some specialized tests need to be sent to Lab Corp and are not quickly available.
In the village, RST, Urine Dips, Hgb, HCG urine and glucose finger sticks are available. They can draw most labs and send them out to Bethel.
For PAPs, we are now doing liquid based, Sure Path. Twist the brush for several seconds on the cervix and then swish in the bottle, then pulling off the brush and leaving it in there. See the desk clerk on how to order the liquid PAP. We are doing Reflex high grade HPV only on older patients or those with a history of ASCUS. See the guidelines.
In the Subregional Clinic, there is a lab capability for some of the tests to be done on site, while others are sent to Bethel. The SRC labs use istat equipment for CBC with WBC , Chem 8 A1C, and a quantitative troponin. They use dipsticks for CCUA and the lab techs can do a urine micro and wet preps. RST and RST cultures can be done as well as urine HCGs, hemocults and gastro cults. Comprehensive Chem panels will need the LFTs in which it needs to be sent out but, the basics can be done at the SRC. Also, the TSH, Quant HCG, etc. can be done as well. Some of the SRCs do set up their own urine cultures and RST cultures; others send them to ANMC. Leslie Boelens is the SRC Lab Manager and trains the entire lab techs. For questions about the lab, please contact her at Aniak SRC @ 907-675-4556.
SRC Pharmacy
Our pharmacists are a great resource. There is a main village pharmacist who is located in Bethel. He comes out to the SRCs periodically to check on narcotic logs etc.
SRCs have a limited formulary. Always feel free to ask the pharmacists questions. You can always call the pharmacist in Bethel at 6652. They are always willing to look up things. We do have a limited formulary and the pharmacists will call you if you order something not on the formulary. If you want something not in the formulary you can use a non-formulary request form. If approved, this med will be then filled for 3 months. If at the end of that time you determine that a patient will have to stay on this medication, you will have to work with pharmacy and request that it be added to the formulary.
The Pharmacy and Therapeutics committee meets once a month. All providers are encouraged to participate via the VTC (video conferencing). It meets the fourth Wednesday of the month at 8 a.m. Contact Natasha, the outpatient pharmacist, for more info.
There is an Outpatient Pharmacist who works with our Standing Order Refill Protocol and will refill patients' meds for 1- 6 months while awaiting a visit or lab results. They also do prior authorizations for all meds that are needed. They are also available for comprehensive medication review, dosing, elders with Poly pharmacy and other prior authorization questions.
To find them call, MON-FRI 8:30 a.m.– 5:30 p.m. Phone #: 6377 / 6196. Or page them on the Ambulatory Clinic Pharmacy through on your computer paging system.
SRC RMT
When staffing allows, the SRC NP/PAs do RMT for their SRC catchment villages. The NP/PA reads the CHA encounter and then reviews the CHA patient orders selected in the appropriate power plan. They will then modify the RMT with a plan and statement and send it back to the Health Aides. When SRC staffing is limited the catchment village Health Aides will be instructed to send their RMTs to Bethel.
When a health aide working at an SRC sees a patient that falls outside of their standing orders, scope of practice or comfort level they will consult the SRC NP/PA and also send an RMT to the SRC NP/PA. The NP/PA may examine the patient if needed. They will advise and/or agree with the plan of care, document this on the health aide RMT and make any orders that are necessary. If the patient is complicated, the SRC PA/NP may take over the care of the patient. In that case the encounter will be moved to the NP/PA’s schedule and the NP/PA will make a power note in RAVEN.
From the catchment villages, if a patient needs a medication to be sent from the Bethel pharmacy, the medication should be ordered from the MENU on the left of the screen, ORDERS tab, click add, then check the correct diagnosis (add diagnosis if necessary), search Ambulatory (Meds as Rx). When you have located the right drug fill in the blanks as needed and in the note to pharmacy indicate “mail to” erase “pick up.”
Eye and Dental RMTS are sent to the respective Eye Doc and Dental proxy boxes.
CPP (Chronic Pediatric Patients) RMT: Health Aides in catchment villages or in a SRC seeing a CPP patient should send the RMT to the Peds/CPP RMT proxy box and get consultation directly from the pediatrician. RMT should not also be sent to the SRC PA/NP (it s confusing when RMT’s are sent to both). However, in the SRC, if the CPP patient is significantly ill; the SRC health aide wants a direct hands-on evaluation; or if there is consideration of transfer to Bethel, then the SRC PA/NP should be notified so they can examine the patient. If the patient is significantly ill, the case will be taken over by the PA/NP who will directly consult with the on-call Pediatrician. In this case, the health aides should send that CPP RMT to the SRC PA/NP to make a note that the patient was examined by the PA/NP and care was assumed.
SRC PA/NPs should feel free to consult "peds on call" about any CPP encounters they are concerned about and/or forward any CPP encounters to the SRC pediatricians that they feel would help the pediatricians with ongoing management or care of these patients.
Urgent or emergency RMT/Consultation: please page the ward doc or night float doctor on call for immediate advice and assistance. Page the pediatrician on call for help and advice for all CPP patients or any other pediatric patients that you would like assistance with.
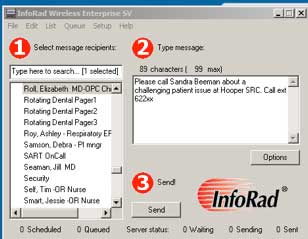
If you need the pediatrician on call or want to page a specific provider, you may also page them directly from your RAVEN desk top:
Open the text paging icon
Select ‘On Call-Pediatrics’ or the provider you are trying to reach and type in a brief message. Say who you are, where you are from and how to reach you. Make sure you identify if it is an emergency. If you do not hear back shortly, try paging again through the operator.
**If no SRC NP/PA is available,
When SRC PA/NP providers are not available catchment area health aides will send routine encounters to RAVEN RMT through the Yukon, Kusko and Peds/CPP RMT Proxy boxes.
For emergency patients who may need medevac or immediate attention in Bethel, health aides will have the operator place an urgent or emergency page to the ward doctor and send the RMT to Emergency/NW Proxy box.
For emergency CPP patients, health aides will have the operator place an urgent or emergency page to the ward doctor and send the RMT to Peds/CPP RMT Proxy box.
For more details on how to do RMT in RAVEN, etc. see RMT Section Link
SRC Village Trips
SRC village trips are usually 2- 4 days. You can order supplies ahead of time by scanning the order to the Club Doc Admin Assistant in Bethel and the supplies can be sent out with you. Alternatively you can bring them from your clinic. Meds can be ordered from the pharmacy and also sent ahead of time. Please let the village know when you will be coming. Upon your return, fill out the attached village trip report. It can be sent electronically by contacting Molly Billy 543-6687.
For detailed information-please see village trips section in the Outpatient Medicine Section
This category currently contains no pages or media.