Abscess Incision and Drainage (I&D): Difference between revisions
From Guide to YKHC Medical Practices
No edit summary |
|||
| Line 11: | Line 11: | ||
===Resources/References=== | ===Resources/References=== | ||
* [https://www.nejm.org/doi/full/10.1056/NEJMvcm071319] | |||
* [[Skin and Soft Tissue Infection]] (YKHC Common/Unique Diagnoses) | * [[Skin and Soft Tissue Infection]] (YKHC Common/Unique Diagnoses) | ||
* [[media:SSTI.pdf|Skin and Soft Tissue Infection YKHC Clinical Guideline]] | * [[media:SSTI.pdf|Skin and Soft Tissue Infection YKHC Clinical Guideline]] | ||
[[Common ED Procedures]] | [[Common ED Procedures]] | ||
Revision as of 01:17, 7 October 2020
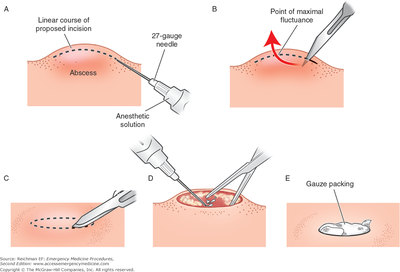
Small abscesses may be drained via needle decompression however most abscesses seen in the emergency room benefit from scalpel incision and drainage.
- Although incision and drainage is not a sterile procedure and does not require sterile technique, typically skin is cleansed with chlorhexidine or povidone-iodine prior to placement of a field block with lidocaine or bupivacaine (step A in image).
- Use a scalpel with a #11 blade to make an incision into the abscess pocket and loculations are bluntly dissected with forceps or wound probe (step B-D).
- While small abscesses may be allowed to drain on their own, most abscesses warranting I&D benefit from packing with either plain gauze, iodoform gauze or a drain (step E).
- Large abscesses may require two incisions to be made and placement of a through Dermastent or penrose drain.
- All purulent drainage should be sent for wound culture to guide antibiotic therapy.
- Per YKHC guidelines abscesses with >/= 10 cm of cellulitis should be covered with antibiotics.
- If there is concern for deep abscesses formal or bedside US may assist in evaluation.
Resources/References
- [1]
- Skin and Soft Tissue Infection (YKHC Common/Unique Diagnoses)
- Skin and Soft Tissue Infection YKHC Clinical Guideline