Adrenal Crisis-Congenital Adrenal Hyperplasia (CAH): Difference between revisions
From Guide to YKHC Medical Practices
(Created page with "Acute adrenal crisis presents as vomiting, diarrhea, dehydration, hypotension and shock. Crisis can be precipitated by illness, trauma and hyperthermia. *'''''If you get a ca...") |
|||
| (8 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
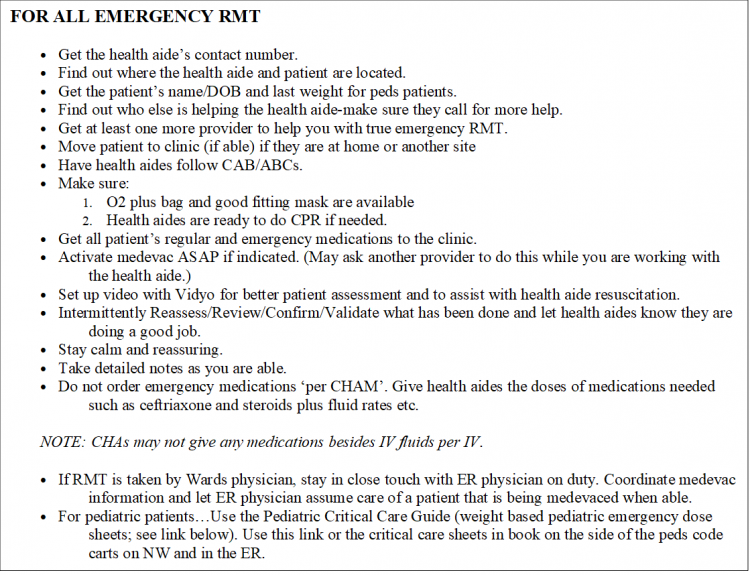
[[image:All Emergency RMT.png|750px]] | |||
[[media:pediatric critical care guide.pdf|Pediatric Critical Care Guide]] | |||
----- | |||
Acute adrenal crisis presents as vomiting, diarrhea, dehydration, hypotension and shock. Crisis can be precipitated by illness, trauma and hyperthermia. | Acute adrenal crisis presents as vomiting, diarrhea, dehydration, hypotension and shock. Crisis can be precipitated by illness, trauma and hyperthermia. | ||
* | |||
* | ==Adult Adrenal Crisis== | ||
*If the | Shock, with hypotension, hypovolemia and possible nonspecific symptoms such as anorexia, nausea, vomiting, abdominal pain, weakness, fatigue, lethargy, fever, confusion, or coma | ||
[[Practicing Medicine in Bush Alaska—Some ABCs#Congenital Adrenal Hyperplasia (CAH)| | |||
*Establish intravenous access with a large-gauge needle. | |||
*Get accucheck glucose and give instaglucose 15-20 gms (1 tube) if needed. Repeat every 15 minutes until symptoms have resolved and glucose is >60. | |||
*Infuse 2 to 3 liters of saline as quickly as possible. | |||
*Give dexamethasone 4 mg IM. | |||
*Continue NS IV fluid hydration | |||
*Continue hemodynamic monitoring and glucose measurement q1h until medevac arrives to avoid fluid overload and recurrent hypoglycemia | |||
==Pediatric Adrenal Crisis with Hypopit/Congenital Adrenal Hyperplasia== | |||
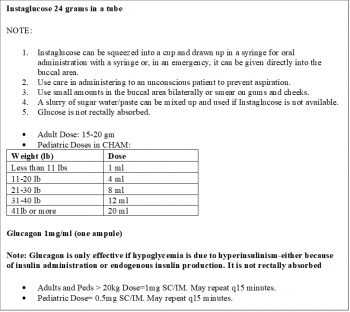
[[file:instaglucose-sb.png|right|350px]] | |||
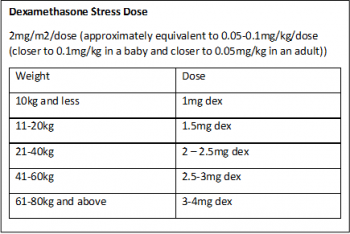
[[file:Dexamethasone_Stress_Dose.png|right|350px]] | |||
Shock, with hypotension, hypovolemia and possible nonspecific symptoms such as anorexia, nausea, vomiting, abdominal pain, weakness, fatigue, lethargy, fever, confusion, or coma | |||
*Establish intravenous access. | |||
*Get accucheck glucose. If glucose result is unknown (ie machine not working), low or undetectable give instaglucose per table. Repeat glucose 15min after giving the glucose gel to confirm that it has normalized | |||
*Give 20ml/kg NS bolus quickly as possible. | |||
*Give dexamethasone IM per table, prescribed home emergency solucortef dose IM or give solucortef per table below (see [https://www.chop.edu/video/solu-cortef-emergency-injection Solu-cortef Emergency Injection] video) | |||
*Monitor hemodynamics, BP and glucose q1h until medevac arrives. | |||
*Continue 1.5 x maintenance NS IV | |||
*Use supportive measures as needed | |||
[[Practicing Medicine in Bush Alaska—Some ABCs#Congenital Adrenal Hyperplasia (CAH)|YKHC Wiki CAH page]] | |||
<br/>[[Emergency RMT Scenarios and Responses]] | |||
Latest revision as of 17:54, 14 December 2020
Acute adrenal crisis presents as vomiting, diarrhea, dehydration, hypotension and shock. Crisis can be precipitated by illness, trauma and hyperthermia.
Adult Adrenal Crisis
Shock, with hypotension, hypovolemia and possible nonspecific symptoms such as anorexia, nausea, vomiting, abdominal pain, weakness, fatigue, lethargy, fever, confusion, or coma
- Establish intravenous access with a large-gauge needle.
- Get accucheck glucose and give instaglucose 15-20 gms (1 tube) if needed. Repeat every 15 minutes until symptoms have resolved and glucose is >60.
- Infuse 2 to 3 liters of saline as quickly as possible.
- Give dexamethasone 4 mg IM.
- Continue NS IV fluid hydration
- Continue hemodynamic monitoring and glucose measurement q1h until medevac arrives to avoid fluid overload and recurrent hypoglycemia
Pediatric Adrenal Crisis with Hypopit/Congenital Adrenal Hyperplasia
Shock, with hypotension, hypovolemia and possible nonspecific symptoms such as anorexia, nausea, vomiting, abdominal pain, weakness, fatigue, lethargy, fever, confusion, or coma
- Establish intravenous access.
- Get accucheck glucose. If glucose result is unknown (ie machine not working), low or undetectable give instaglucose per table. Repeat glucose 15min after giving the glucose gel to confirm that it has normalized
- Give 20ml/kg NS bolus quickly as possible.
- Give dexamethasone IM per table, prescribed home emergency solucortef dose IM or give solucortef per table below (see Solu-cortef Emergency Injection video)
- Monitor hemodynamics, BP and glucose q1h until medevac arrives.
- Continue 1.5 x maintenance NS IV
- Use supportive measures as needed