Helicobacter pylori in Alaska Natives: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
===International Multi-Disciplinary Working Group=== | ===International Multi-Disciplinary Working Group=== | ||
In 2016 an international, multi-disciplinary working group, including representative from the CDC Arctic Research Center and Alaska Native Tribal Health Consortium, published an Expert Commentary<ref>McMahon BJ, Bruce MG, Koch A, et al. The diagnosis and treatment of Helicobacter pylori infection in Arctic regions with a high prevalence of infection: Expert Commentary. Epidemiology and Infection. 2016;144(2):225-233. doi:10.1017/S0950268815001181. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4697284/pdf/S0950268815001181a.pdf '''Free PMC Article'''].</ref> which thoroughly reviewed the epidemiology, associated clinical syndromes, diagnosis, and treatment of H. pylori in high prevalence populations. Some of the key findings/recommendations | In 2016 an international, multi-disciplinary working group, including representative from the CDC Arctic Research Center and Alaska Native Tribal Health Consortium, published an Expert Commentary<ref>McMahon BJ, Bruce MG, Koch A, et al. The diagnosis and treatment of Helicobacter pylori infection in Arctic regions with a high prevalence of infection: Expert Commentary. Epidemiology and Infection. 2016;144(2):225-233. doi:10.1017/S0950268815001181. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4697284/pdf/S0950268815001181a.pdf '''Free PMC Article'''].</ref> which thoroughly reviewed the epidemiology, associated clinical syndromes, diagnosis, and treatment of H. pylori in high prevalence populations. Some of the key findings/recommendations were: | ||
* ''Screening or testing for H. pylori infection for the routine evaluation of dyspepsia or other gastrointestinal symptoms, whether utilizing serology, UBT or other techniques, is not clinically useful or supported by clinical evidence for high prevalence populations such as in the Arctic.'' | * ''Screening or testing for H. pylori infection for the routine evaluation of dyspepsia or other gastrointestinal symptoms, whether utilizing serology, UBT or other techniques, is not clinically useful or supported by clinical evidence for high prevalence populations such as in the Arctic.'' | ||
| Line 11: | Line 11: | ||
'' | '' | ||
* Evidence supports treatment of H. pylori in | * Evidence supports treatment of H. pylori only in these situations: | ||
:# Duodenal ulcer | :# Duodenal ulcer | ||
:# Gasgric ulcer | :# Gasgric ulcer | ||
| Line 25: | Line 25: | ||
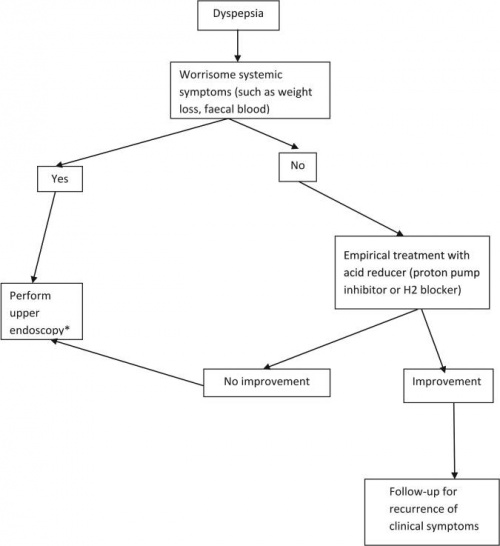
[[File:IWG Figure-1.jpg| | [[File:IWG Figure-1.jpg|500px|border|center|Algorithm for management of dyspepsia in regions with high prevalence (>60% population infected) of Helicobacter pylori infection.]] | ||
| Line 33: | Line 33: | ||
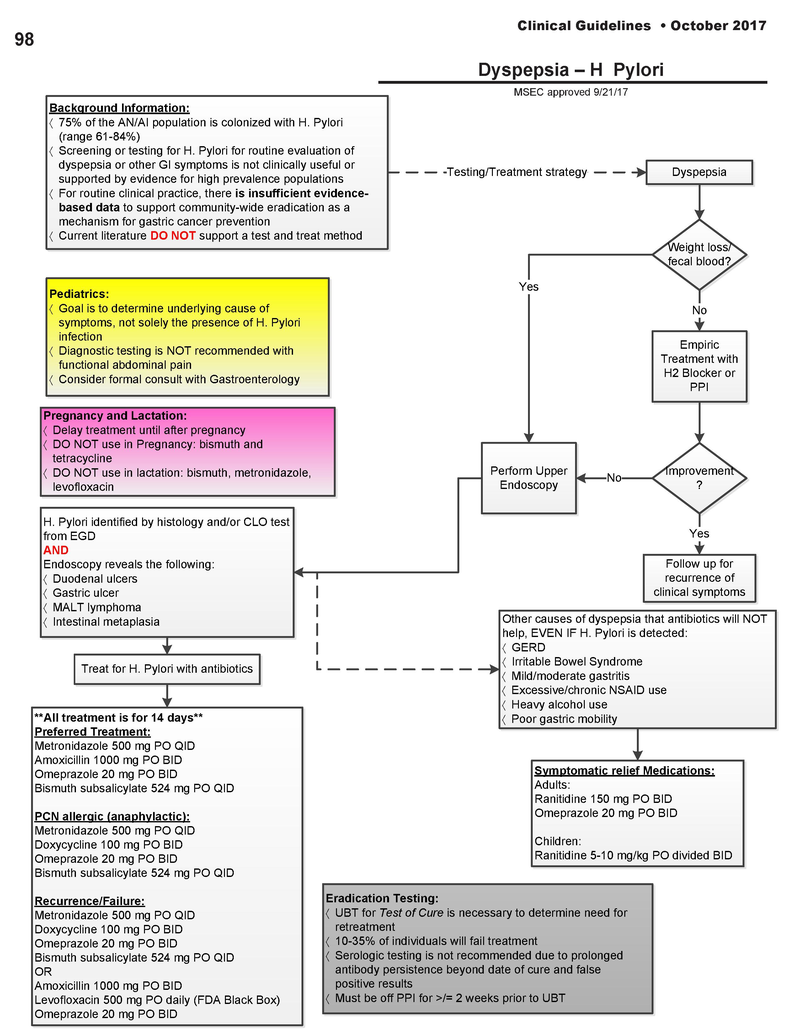
[[File:Guidelines2017 H-pylori.pdf| | [[File:Guidelines2017 H-pylori.pdf|800px|border|center|YKHC/ANMC Guideline]] | ||
===CDC Cultures and Sensitivities=== | |||
YKHC participates in a CDC funded program to monitor H. pylori drug sensitivities in rural, high prevalence Alaska communities. | |||
Revision as of 01:19, 13 October 2017
Helicobacter pylori is present in the stomach of the majority of adult Alaska Natives, with a similar prevalence in other circumpolar indigenous peoples. The high prevalance, high drug resistance rate, and high reinfection rate present unique challenges for management of Alaska Natives with upper GI symptoms.
International Multi-Disciplinary Working Group
In 2016 an international, multi-disciplinary working group, including representative from the CDC Arctic Research Center and Alaska Native Tribal Health Consortium, published an Expert Commentary[1] which thoroughly reviewed the epidemiology, associated clinical syndromes, diagnosis, and treatment of H. pylori in high prevalence populations. Some of the key findings/recommendations were:
- Screening or testing for H. pylori infection for the routine evaluation of dyspepsia or other gastrointestinal symptoms, whether utilizing serology, UBT or other techniques, is not clinically useful or supported by clinical evidence for high prevalence populations such as in the Arctic.
- When treatment is employed, treatment should consist of regimens that have evidence of high efficacy after taking into consideration the antimicrobial resistance patterns in the region.
- Evidence supports treatment of H. pylori only in these situations:
- Duodenal ulcer
- Gasgric ulcer
- MALT lymphoma
- When the goal is treatment of dyspepsia in patients from populations where H. pylori is highly prevalent, there is moderate evidence that H. pylori therapy should be undertaken only when there is endoscopic or histopathological confirmation of a condition associated with improvement following elimination of H. pylori, such as peptic ulcer disease.
- There is insufficient evidenced-based data to support the H. pylori test-and-treat strategy in patients with non-specific dyspepsia.
Based upon these conclusions, the Working Group proposed the following algorithm for management of dyspepsia in high prevalence (>60%) populations:
YKHC/ANMC Guideline
In September 2017, the YKHC Medical Staff Executive Committee adopted/approved the ANMC H. pylori guideline, which is based upon the International Multi-Disciplinary Working Group findings and recommendations:
CDC Cultures and Sensitivities
YKHC participates in a CDC funded program to monitor H. pylori drug sensitivities in rural, high prevalence Alaska communities.
Pediatric Considerations
Dr Hermann's input will go here.
References
- ↑ McMahon BJ, Bruce MG, Koch A, et al. The diagnosis and treatment of Helicobacter pylori infection in Arctic regions with a high prevalence of infection: Expert Commentary. Epidemiology and Infection. 2016;144(2):225-233. doi:10.1017/S0950268815001181. Free PMC Article.