High-sensitivity Troponin-T
see Acute Coronary Syndrome Wiki Supplement Page for other information associated with Acute Coronary Syndrome
On November 12, 2019, the Yukon-Kuskokwim Delta Regional Hospital (YKDHR) switched cardiac troponin assay to the Roche Diagnostics Elecsys® Troponin T Gen 5 STAT. This is a high-sensitivity fifth-generation cardiac troponin assay. Details are available in the manufacturer's package insert.
Cardiac troponin assays measure the concentration of either troponin-T or troponin-I. Both high-sensitivity and traditional troponin assays measure the exact same molecule, but high-sensitivity assays measure much more precisely and at much lower concentrations. The high-sensitivity and traditional assays can be distinguished by the units in which they are reported: high-sensitivity assays are reported in ng/L whereas the traditional assays are reported in ng/mL.
- Conversion between the results can be done by moving the decimal point three places: a traditional concentration of 0.4 ng/mL is equivalent to a high-sensitivity concentration of 400 ng/L, and a high-sensitivity concentration of 14 ng/L is equivalent to a traditional concentration of 0.014 ng/mL. This latter conversion illustrates that the high-sensitivity assays accurately measure concentrations which are two orders of magnitude lower than the assay we were previously using.
Though high-sensitivity troponin assays have been used in Europe and Canada since approximately 2009, the first U.S. FDA approval occurred in 2017.
NOTE: The information below is not a guideline, but rather excerpts and links intended to augment and/or help develop clinical judgement.
Definition
To qualify as high-sensitivity (or highly-sensitive), a cardiac troponin assay must be able to detect a level of cardiac troponin in >50% of normal individuals.[1] This means that the majority of patients without cardiac ischemia will have a detectable level of cardiac troponin. This has substantial implications for how clinicians conceptualize and interpret cardiac troponin levels.
Statistical/Epidemiological Properties
Delta (Δ) versus Level
Troponin Delta
Troponin Level
Level Cutoffs
Hs-cTnT is considered "positive" when above the gender-specific 99th percentile URL (upper reference range). Per eMail from Scott Cox (YKDHR Director of Diagnostic Services) on 11/10/2019, the following cutoff are recommended for our assay:
| Women | >= 14 ng/L |
| Men | >= 22 ng/L |
Per the ACC white paper (see below):
- A single Hs-cTnT >= 100 ng/L is diagnostic of AMI (in the appropriate clinical context).
- When chest pain has been present for >= 3 hours, a single Hs-cTnT < 6 ng/L has been reported to rule out AMI with essentially 100% negative predictive value.
Diagnostic Algorithms
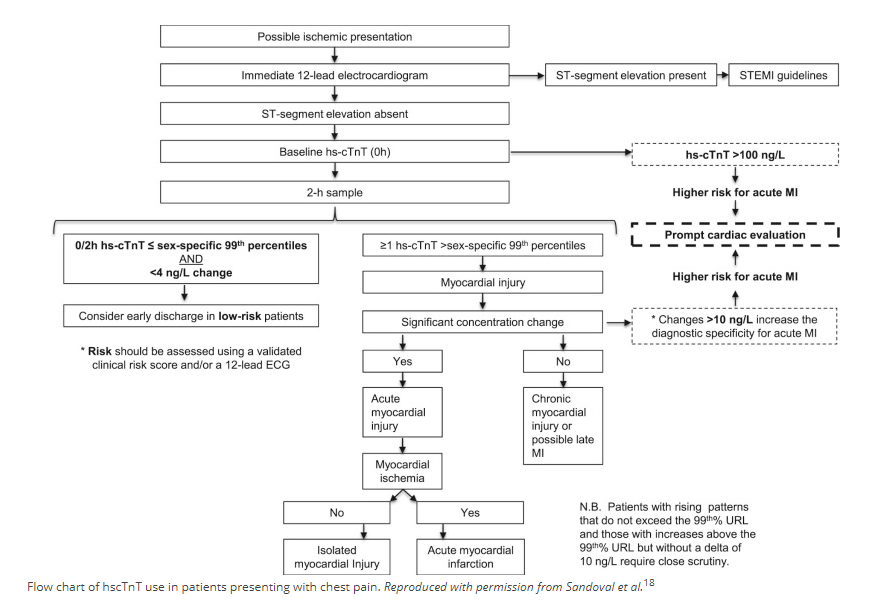
ACC
The following diagnostic algorithm has been proposed for high-sensitivity cardiac troponin-T by the ACC (American College of Cardiology), though they caution that "The safety of this approach is currently unclear":[1]
UTSW/Parkland
The algorithm used by University of Texas Southwestern Medical Center is shown for illustrative purposes in an ACEP Webinar (see below, page 16):
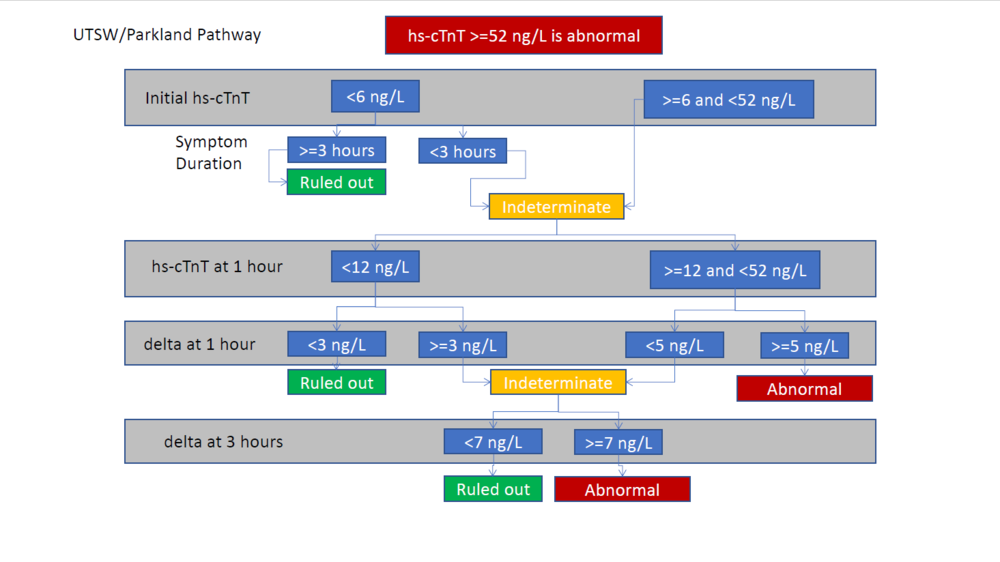
Note that this algorithm does not include risk stratification, such as with the HEART score. Yet the same Webinar contains other algorithms which separate out Hs-cTnT and call the risk stratification a HEAR score (or "modified-HEART" score) and guide diagnosis/management based upon different combinations of Hs-cTnT and HEAR values. Yet other algorithms in the same Webinar recommend skipping risk stratification in those who have low- or high-risk EKG/Hs-cTnT results and only risk stratifying those with intermediate-risk EKG/Hs-cTnT results.
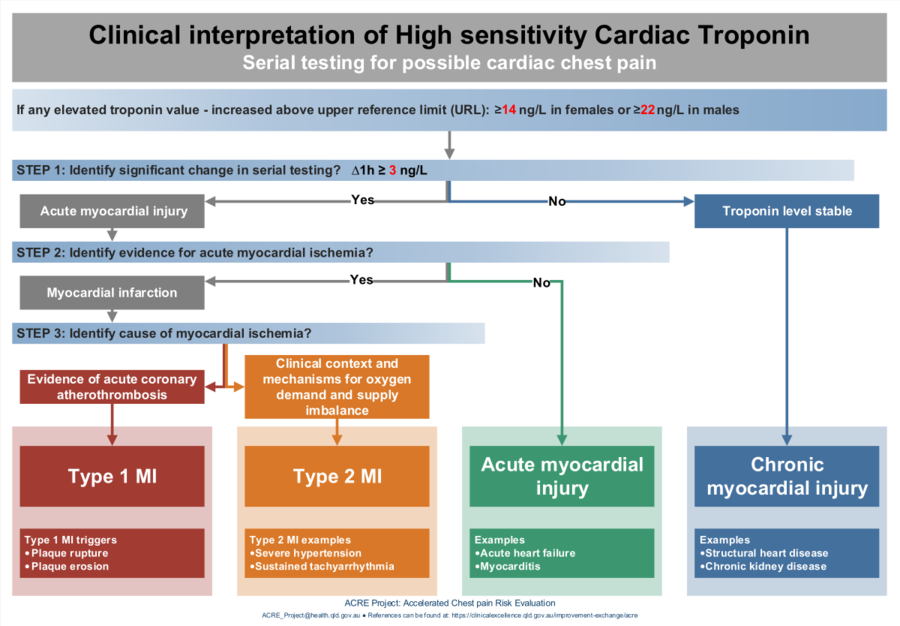
Australian ACRE Project
This diagnostic algorithm guides the user to one of four etiologies for HS-cTnT elevation:
- Type-1 MI
- Type-2 MI
- Acute myocardial injury
- Chronic myocardial injury
However, users will note that the following two terms are used without definition:
- Evidence for acute myocardial ischemia
- Evidence of acute coronary atherothrombosis
Per recommendation of the author, this algorithm has been edited to contain the cutoffs specific to our lab/assay:
The original PDF is available here (archived)
Helpful Links
ACC (American College of Cardiology)
- High-Sensitivity Cardiac Troponin in the Evaluation of Possible AMI (July 16, 2018)
- SUMMARY: Fourth Universal Definition of Myocardial Infarction (Aug 25, 2018)
ACEP
- Webinar: Incorporating High-Sensitivity Troponin into Your ED
- Critical Issues in the Evaluation and Management of Emergency Department Patients with Suspected Non–ST-Elevation Acute Coronary Syndromes (Jun 2018)
MD Calc
ACEPNow Articles
- 03-19-2019: High Sensitivity Cardiac Troponin Tests for Acute Myocardial Infarction May be Flawed
- 09-18-2019: Chest-Pain Patients and High-Sensitivity Troponin Tests: the New Frontier
PodCasts
- 02-20-2020: EMCrit #266: High Sensitivity Troponins with Louise Cullen (Duration: 26:04) Archived
- 01-18-2020: SGEM #280: THIS OLD HEART OF MINE AND TROPONIN TESTING (Duration: 30:10) Archived
- 07-30-2019: Emergency Medicine Cases (Ep 128) Low Risk Chest Pain and High Sensitivity Troponin – A Paradigm Shift (Duration: 1:34:36) Archived
High-sensitivity troponin Myths versus Reality
Myths:
- more patients will undergo catheterization
- ED stays will be longer
- there will be fewer ED discharges
- there will be more stress tests
FACT: the APACE trial showed that adoption of a high-sensitivity troponin assay was associated with no change in the number of catheterizations, decreased "normal cath" results, shorter ED stays, more ED discharges, and fewer stress tests.[2]
FACT: Across numerous trials, increasing troponin sensitivity has shown a dose-response relationship with increased ED discharges.
Controversies
Recommended 99% URL Cutoffs
Mariathas el al (Mar 2019)
- In March 2019 Mariathas el al. reported in the BMJ[3] that they found a very different distribution and 99% ULR when they analyzed 20,000 consecutive blood samples collected in all settings (outpatient, ED, inpatient, etc.) drawn for any reason in a large UK hospital. Overall, over five percent of patients had a troponin-I result greater than the manufacturer recommended 99% cutoff of 40 ng/L, and far too many older patients and inpatients exceed this recommended cutoff:
- The implications of such a degree of variation are substantial, and may indicate that individual institutions need to calculate their own age-adjusted 99% cutoffs in order to obtain the intended outcomes. Additionally, clinicians likely need to integrate patient age and clinical context into their interpretation of hs-Tn levels. Though hs-Tn's have been shown to improve outcomes when evaluating acute chest pain in emergency departments, there is no data to indicate that diagnosing myocardial injury in 15% of medical ward patients, 20% of older persons, and 40% of ICU patients will lead to patient-important improvements.
- However... readers are strongly encouraged to read all seven of the responses. In particular, Paul Collinson makes a strong argument that the authors are mis-interpreting their data because they are including a substantial number of UNhealthy individuals (i.e with CHF, CKI, etc.), whereas the appropriate cutoffs are [by definition] derived from healthy individuals. All of the responses are thoughtful, and both the article and the responses provide interesting thoughts about troponin levels and binary versus Bayesian interpretation of results.
The significance of Myocardial Injury
Acute
- There is no standard-of-care workup for this finding in the absence of myocardial ischemia. Can it be attributed to a tachyarrythmia, sepsis, etc? Or should a PE be ruled-out? Does it mandate an echocardiogram?
Chronic
- This is certainly not amenable to ED intervention. Again, it is not clear what the standard-of-care disposition of this finding will be.
Definitions
- Myocardial injury
- Elevated cardiac troponin values (cTn) with at least one value above the 99th percentile upper reference limit (URL).[4]
- Acute myocardial injury
- Myocardial injury with a rise and/or fall of cTn values.[4]
- Acute myocardial infarction (types 1, 2 and 3 MI)
- Acute myocardial injury and at least one of the following:[4]
- - Symptoms consistent with acute coronary occlusion;
- - New ischaemic ECG changes;
- - Development of pathological Q waves;
- - Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischaemic aetiology;
- - Identification of a coronary thrombus by angiography or autopsy (not for type 2 or 3 MIs).
- Acute myocardial injury and at least one of the following:[4]
References
- ↑ 1.0 1.1 High-Sensitivity Cardiac Troponin in the Evaluation of Possible AMI. American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2018/07/16/09/17/high-sensitivity-cardiac-troponin-in-the-evaluation-of-possible-ami. Accessed December 3, 2019.
- ↑ Twerenbold R, Jaeger C, Rubini Gimenez M, et al. Impact of high-sensitivity cardiac troponin on use of coronary angiography, cardiac stress testing, and time to discharge in suspected acute myocardial infarction. Eur Heart J. 2016;37(44):3324-3332. doi:10.1093/eurheartj/ehw232
- ↑ Mariathas M, Allan R, Ramamoorthy S, et al. True 99th centile of high sensitivity cardiac troponin for hospital patients: prospective, observational cohort study. BMJ. 2019;364:l729. doi:10.1136/bmj.l729
- ↑ 4.0 4.1 4.2 Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Journal of the American College of Cardiology. 2018;72(18):2231-2264. doi:DOI: 10.1016/j.jacc.2018.08.1038
![Overall distribution. (Note that the vertical axis is logarithmic, which substantially [over]emphasizes the appearance of the frequency of the higher troponin levels.)](/images/thumb/1/13/Hs-TnI_histogram_Mariathas_2019.jpg/96px-Hs-TnI_histogram_Mariathas_2019.jpg)