Seizures RMT: Difference between revisions
From Guide to YKHC Medical Practices
| Line 33: | Line 33: | ||
* If seizure does not resolve or is prolonged, activate a medevac ASAP. | * If seizure does not resolve or is prolonged, activate a medevac ASAP. | ||
* Place IV if possible and give NS bolus as appropriate. Remember, hyponatremia is another reversible cause of status epilepticus; giving a NS bolus may help stop the seizure. | * Place IV if possible and give NS bolus as appropriate. Remember, hyponatremia is another reversible cause of status epilepticus; giving a NS bolus may help stop the seizure. | ||
* If a patient has seized for more than 5-10 minutes, be prepared to start with either the patient’s rectal Diastat prescription or the anti-seizure medications in box | * If a patient has seized for more than 5-10 minutes, be prepared to start with either the patient’s rectal Diastat prescription or the anti-seizure medications in the box below. | ||
* REMEMBER…the longer a patient seizes the harder it is to break the seizure. | * REMEMBER…the longer a patient seizes the harder it is to break the seizure. | ||
* Before giving benzodiazepines or phenobarbital, make sure the health aide has obtained a good fitting bag and mask and is ready to provide assisted ventilation with bag-mask-valve device to support the patient if the patient becomes apneic. Diazepam can be repeated as often as every 5-15 minutes. | * Before giving benzodiazepines or phenobarbital, make sure the health aide has obtained a good fitting bag and mask and is ready to provide assisted ventilation with bag-mask-valve device to support the patient if the patient becomes apneic. Diazepam can be repeated as often as every 5-15 minutes. | ||
* Ask for inpatient pharmacist assistance if needed. | * Ask for inpatient pharmacist assistance if needed. | ||
[[file:midazdose-sb.png]] | |||
* Take notes with times, medications given, interventions done, and responses. | * Take notes with times, medications given, interventions done, and responses. | ||
* Get Vidyo set up for monitoring if not done already if seizure management is ongoing. | * Get Vidyo set up for monitoring if not done already if seizure management is ongoing. | ||
Revision as of 00:33, 11 May 2019
----------------------------------------------------
FOR ALL EMERGENCY RMT
- Get the health aide’s contact number.
- Find out where the health aide and patient are located.
- Get the patient’s name/DOB and last weight for peds patients.
- Find out who else is helping the health aide-make sure they call for more help.
- Get at least one more provider to help you with true emergency RMT.
- Move patient to clinic if they are at home or another site.
- Have health aides follow CAB/ABCs.
- Make sure:
- O2 plus bag and good fitting mask are available.
- Health aides are ready to do CPR if needed.
- Get all patient’s regular and emergency medications to the clinic.
- Activate medevac ASAP if indicated.
- Set up video with Vidyo for better patient assessment and to assist with health aide resuscitation.
- Intermittently Reassess/Review/Confirm/Validate what has been done and let health aides know they are doing a good job.
- Stay calm and reassuring.
- Take detailed notes as you are able.
- Do not order emergency medications ‘per CHAM’. Give health aides the doses of medications needed such as ceftriaxone and steroids plus fluid rates etc.
- NOTE: CHAs may not give any medications besides IV fluids per IV.
- For pediatric patients…Use the Pediatric Critical Care Guide (weight based pediatric emergency dose sheets). Use this link or the critical care sheets in book on the side of the peds code carts on NW and in the ER.
- If RMT is taken by Wards physician, stay in close touch with ER physician on duty. Coordinate medevac information and let ER physician assume care of a patient that is being medevaced when able.
-----------------------------------------
Seizure Evaluation and Treatment
- Determine if the patient is still seizing—there may no longer be tonic-clonic movements, but patient may be stiff, have fine tremors, eye deviation (or nystagmus), poor O2 sats, etc.
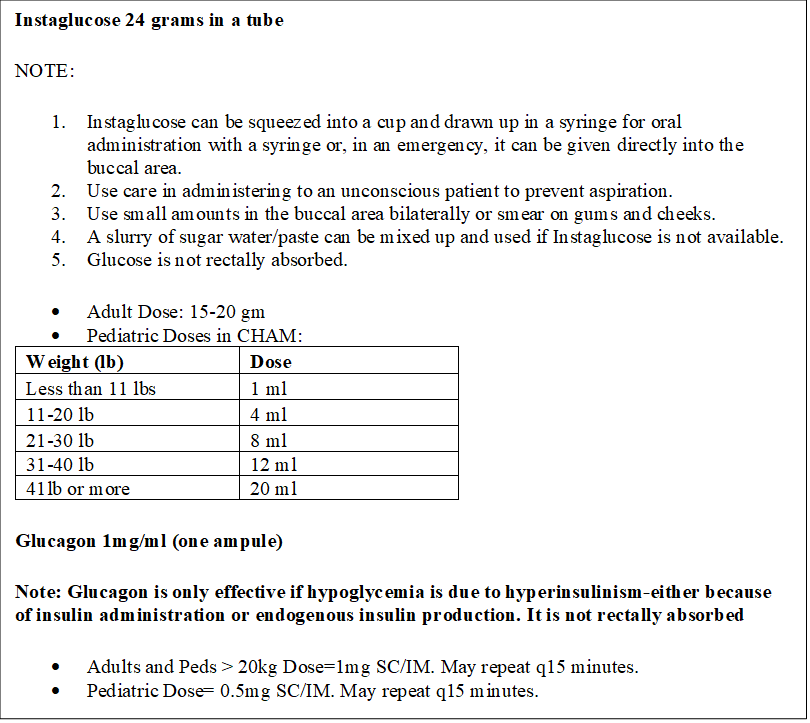
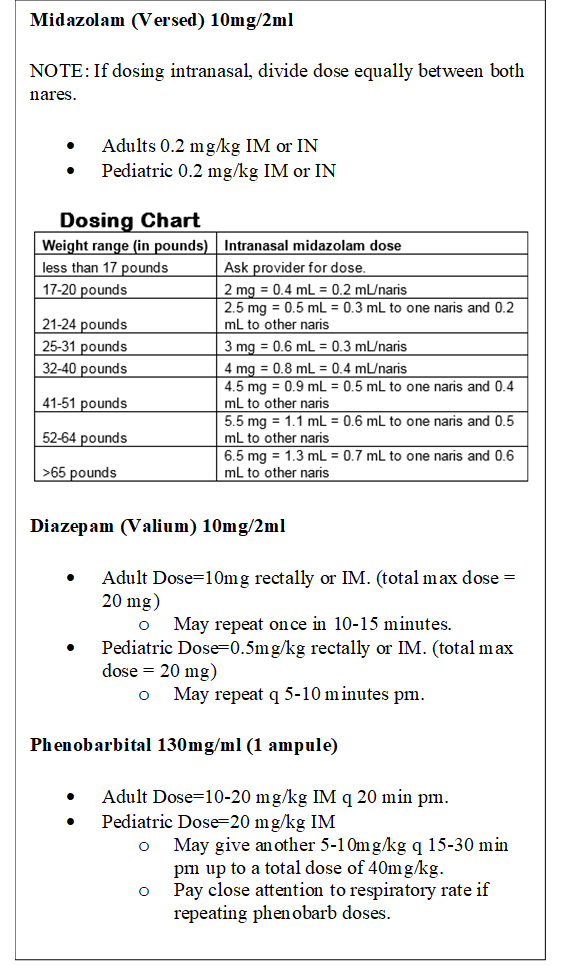
- Have a health aide get Instaglucose, Midazolam, Diazepam, and Phenobarbital out of the village clinic lock box and ready for administering.
- Have Bag and Mask ready especially for repeat doses of sedating medications
- Get an Accucheck glucose ASAP (low glucose is a reversible cause of seizures) and continue to monitor glucose.
- For low or undetectable blood glucose--see village medications doses in boxes to the right.
- If seizure does not resolve or is prolonged, activate a medevac ASAP.
- Place IV if possible and give NS bolus as appropriate. Remember, hyponatremia is another reversible cause of status epilepticus; giving a NS bolus may help stop the seizure.
- If a patient has seized for more than 5-10 minutes, be prepared to start with either the patient’s rectal Diastat prescription or the anti-seizure medications in the box below.
- REMEMBER…the longer a patient seizes the harder it is to break the seizure.
- Before giving benzodiazepines or phenobarbital, make sure the health aide has obtained a good fitting bag and mask and is ready to provide assisted ventilation with bag-mask-valve device to support the patient if the patient becomes apneic. Diazepam can be repeated as often as every 5-15 minutes.
- Ask for inpatient pharmacist assistance if needed.
- Take notes with times, medications given, interventions done, and responses.
- Get Vidyo set up for monitoring if not done already if seizure management is ongoing.
- The second line medication will sometimes need be phenobarbital IM. For adults, the dose of IM phenobarb may exhaust the entire village supply!
- If you think there is any chance that the seizure is from infection-Don’t forget to give Ceftriaxone.
- Any emergency RMT requiring a medevac needs to be communicated to the ER physician and PTO completed.